 Researchers at the University of Oxford have begun enrolling subjects in a phase 2/3 clinical trial of AstraZeneca-partnered COVID-19 vaccine AZD1222. The next stage of the program, which follows a 1,000-subject phase 1, is set to enroll 10,260 people in the U.K. to generate results to support the first shipmentsto customers in September.
Researchers at the University of Oxford have begun enrolling subjects in a phase 2/3 clinical trial of AstraZeneca-partnered COVID-19 vaccine AZD1222. The next stage of the program, which follows a 1,000-subject phase 1, is set to enroll 10,260 people in the U.K. to generate results to support the first shipmentsto customers in September.
AZD1222, the recombinant adenovirus vaccine that originated in Oxford, entered the clinic shortly after another candidate vaccine being developed by Moderna, a German-based bio-tech startup. The initiation of the phase 1 trial marked the start of a large, significantly truncated development program plotted out by researchers at the University of Oxford, who have talked up the prospect of making the vaccine available in September.
Work toward that goal is advancing apace on multiple fronts. On the R&D side, the University of Oxford said Friday that it has begun enrolling participants in the phase 2 portion of the program.
The phase 2 will relax the exclusion criteria used in the phase 1, notably by enrolling a small number of children aged 5 to 12 years and adults aged 56 years and older. One cohort will enroll adults aged over 70 years, a demographic that is particularly at risk from the coronavirus. By expanding the age range, the researchers aim to understand how immune response varies across demographics.
Once the vaccine moves into phase 3, the researchers will limit enrollment to people age 18 years and older. Adult participants in the phase 2 and 3 trials will be randomized to receive one or two doses of AZD1222 or a vaccine against meningococcal bacteria that will serve as the control.
The use of an active vaccine as a control is intended to ensure participants are unable to tell whether they received AZD1222 based on side effects such as soreness at the injection site. In the absence of such effects across both groups, participants could determine whether they had received the vaccine and make behavioral changes that skew the results of the study.
Investigators plan to administer the vaccines to participants in the next stage of the study across May and June. Subjects will then attend follow-up visits to provide blood samples that will show whether their immune system has responded to the virus. The researchers will also ask some participants to log any symptoms they feel in the week after vaccination.
Those measures will provide an early look at the safety and immunogenicity of the vaccine, but it will take longer to gauge whether the shot can prevent people from becoming infected with the coronavirus.
The researchers are trying to accelerate that process by enrolling healthcare workers and other people who are more likely to be exposed to the virus. Depending on the extent to which SARS-CoV-2 is present in the U.K., it is expected to take two to six months for enough infections to happen to show whether the vaccine is working.
Neither the university nor AstraZeneca are hanging around to see if that is the case before preparing for widespread use of the vaccine. The phase 2/3 trial is getting underway despite the university being yet to share phase 1 data, and AstraZeneca is already racing to equip itself to ship 1 billion doses.
– Fierce Life Sciences
Q & A: AZD1222 Phase II/III Clinical Trial Explained
 What is the purpose of this research study?
What is the purpose of this research study?
The purpose of this study is to test a new vaccine against COVID-19 in healthy volunteers.
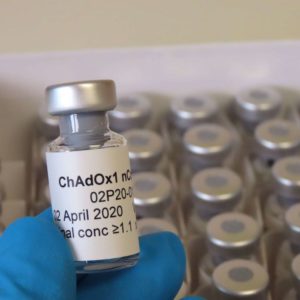
This study aims to assess how well people across a broad range of ages could be protected from COVID-19 with this new vaccine called ChAdOx1 nCoV-19. It will also provide valuable information on safety aspects of the vaccine and its ability to generate good immune responses against the virus.
What is the vaccine being tested?
ChAdOx1 nCoV-19 is made from a virus (ChAdOx1), which is a weakened version of a common cold virus (adenovirus) that causes infections in chimpanzees, that has been genetically changed so that it is impossible for it to grow in humans.
Genetic material has been added to the ChAdOx1 construct, that is used to make proteins from the COVID-19 virus (SARS-CoV-2) called Spike glycoprotein (S). This protein is usually found on the surface of SARS-CoV-2 and plays an essential role in the infection pathway of the SARS-CoV-2 virus. The SARS-CoV-2 coronavirus uses its spike protein to bind to ACE2 receptors on human cells to gain entry to the cells and cause an infection.
By vaccinating with ChAdOx1 nCoV-19, we are hoping to make the body recognise and develop an immune response to the Spike protein that will help stop the SARS-CoV-2 virus from entering human cells and therefore prevent infection.
Has the vaccine been tested on animals?
Our collaborators at Rocky Mountain Laboratories (NIAID/NIH) have conducted a rapid yet thorough investigation and demonstrated good safety and efficacy of a single dose of ChAdOx1 nCoV-19 in the rhesus macaque model that they had previously established. We were able to review the data before vaccinations in the clinical trial were initiated. There are also animal studies underway in Australia and the UK, and the results will be published once those studies are complete.
What does the study involve?
In total this study will enrol up to 10,260 adults and children across the UK.
The phase II part of the study involves expanding the age range of people the vaccine is assessed in, to include a small number of adults and children:
- Aged 56-69
• Aged over 70
• Aged between 5-12 years
For these groups, researchers are assessing the immune response to the vaccine in people of different ages, to find out if there is variation in how well the immune system responds in older people or children.
The phase III part of the study involves assessing how the vaccine works in a large number of people over the age of 18. This group will allow assessment of how well the vaccine works to prevent people from becoming infected with COVID-19.
Adult participants in both the Phase II and Phase III groups will be randomised to receive one or two doses of either the ChAdOx1 nCoV-19 vaccine or a licensed vaccine (MenACWY) that will be used as a ‘control’ for comparison.
What is the MenACWY vaccine?
The MenACWY vaccine is a licensed vaccine against group A, C, W and Y meningococcus which has been given routinely to teenagers in the UK since 2015 and protects against one of the most common causes of meningitis and sepsis. This vaccine is also given as a travel vaccine for high risk countries.
The MenACWY vaccine is being used as an ‘active control’ vaccine in this study, to help us understand participants’ response to ChAdOx1 nCoV-19. The reason for using this vaccine, rather than a saline control, is because we expect to see some minor side effects from the ChAdOx1 nCOV-19 vaccine such as a sore arm, headache and fever. Saline does not cause any of these side effects. If participants were to receive only this vaccine or a saline control, and went on to develop side effects, they would be aware that they had received the new vaccine. It is critical for this study that participants remain blinded to whether or not they have received the vaccine, as, if they knew, this could affect their health behaviour in the community following vaccination, and may lead to a bias in the results of the study.
Who can take part in the study?
| Participants must: | Participants must NOT: |
| Be in one of the relevant age categories | Have tested positive for COVID-19 |
| Be in good health | Be pregnant, intending to become pregnant, or breastfeeding during the study |
| Based in one of the recruiting areas | Have previously taken part in a trial with an adenoviral vaccine or received any other coronavirus vaccines |
Full inclusion and exclusion criteria is available in the participant information sheet.
How will the trial work?
The main focus of the study is to find out if this vaccine is going to work against COVID-19, if it won’t cause unacceptable side effects and if it induces good immune responses. The dose used in this trial was chosen based on previous experiences with other ChAdOx1 based vaccines.
Study participants will not know whether they have received the ChAdOx1 nCoV-19 vaccine until the end of the trial.
To recruit the large number of participants needed for this trial, multiple clinical research sites across the UK are involved in delivering the study. This is a collaborative effort led by the University of Oxford and a full list of our study sites is available on our website. Vaccinations will be taking place across the sites in May and June.
What about after the vaccination?
Some participants will be given an E-diary to record any symptoms experienced for 7 days after receiving the vaccine and if they feel unwell for the following 3 weeks. There is also a weekly survey that participants will be asked to complete about any household exposure to COVID-19.
In order to monitor exposure to COVID-19 in people who do not have symptoms, participants in some areas will be asked to collect swabs at home to be sent to the laboratory for testing.
Following vaccination, participants will attend a series of short follow-up visits. During these visits, the team will check participants’ observations, take a blood sample and review the completed E-diary and questionnaire. These blood samples will be used to assess the immune response to the vaccine.
If participants develop COVID-19 symptoms during the study, they can contact a member of the clinical team, and we will assess them to check whether they have become infected with the virus. If a participant was very unwell, we would call our colleagues in the hospital and ask them to review the volunteer if appropriate.
When will the results be available?
To assess whether the vaccine works to protect from COVID-19, the statisticians in our team will compare the number of infections in the control group with the number of infections in the vaccinated group. For this purpose, it is necessary for a small number of study participants to develop COVID-19. How quickly we reach the numbers required will depend on the levels of virus transmission in the community. If transmission remains high, we may get enough data in a couple of months to see if the vaccine works, but if transmission levels drop, this could take up to 6 months. Recruitment of those who have a higher chance of being exposed to the SARS-CoV-2 virus is being prioritised, such as frontline healthcare workers, frontline support staff and public-facing key workers, in an effort to capture the efficacy data as quickly as possible.
What if it doesn’t work?
A significant proportion of vaccines that are tested in clinical trials don’t work. If we are unable to show that the vaccine is protective against the virus, we would review progress, examine alternative approaches, such as using different numbers of doses, and would potentially stop the programme.
- Courtesy: University of Oxford

